-
Teresa Wilson’s first apartment of her own was a big deal. “She felt like she was gaining more independence. And I think the more she tried to gain that…
-
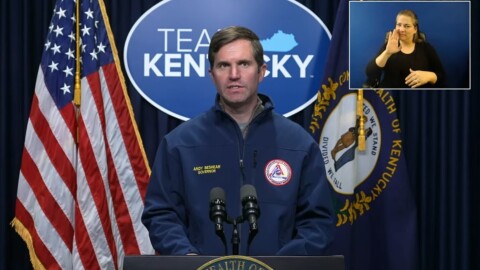
Kentucky continues to see a drop in new COVID-19 cases and positivity rates as the omicron variant appears to loosen its hold on the region. At a news…
-
Staffing shortages continue to cripple some Tennessee hospitals dealing high COVID numbers among patients and their own staff. The pinch is being felt by…
-
COVID hospitalizations are near their record as state officials hope omicron surge is on the declineThe pressure on Kentucky hospitals from the COVID-19 omicron variant is unrelenting. “Hospitalization is near a record high. We are close to the height of…
-
Western Kentucky health departments have scaled back or completely stopped making check-in calls in recent weeks to those who test positive for COVID-19…
-
Some Kentucky hospitals stretched thin by the latest COVID-19 surge are turning to outside help to keep operations flowing. Eleven AmeriCorps volunteers…
-
Kentucky officials continue to report record high COVID-19 cases, but say the peak – of at least the omicron variant – is in sight. At a news conference…
-
Corina Hall remembers looking out her window and watching her car be submerged by water shortly before 4 a.m. on March 1, 2021. Minutes later, water…
-
Kentucky continues to see record COVID-19 cases, which are putting a strain on the state’s hospitals. The state has now surpassed one million cases – with…
-
The COVID-19 pandemic has been especially difficult for young people in high school and college in Kentucky and across the U.S. The threat of illness, the…
-
Patsy Wilkerson and Ashley Rose have a running joke that keeps them chuckling during long days working at Knollwood Manor in Lafayette, Tenn. They’re both…
-
More than a quarter of COVID-19 tests in Kentucky are now coming back positive, and the state is sending more Kentucky National Guard members to help in…